Early Detection of Parkinson’s Disease and Safer Diagnosis by blood markers
Parkinson’s Disease Overview
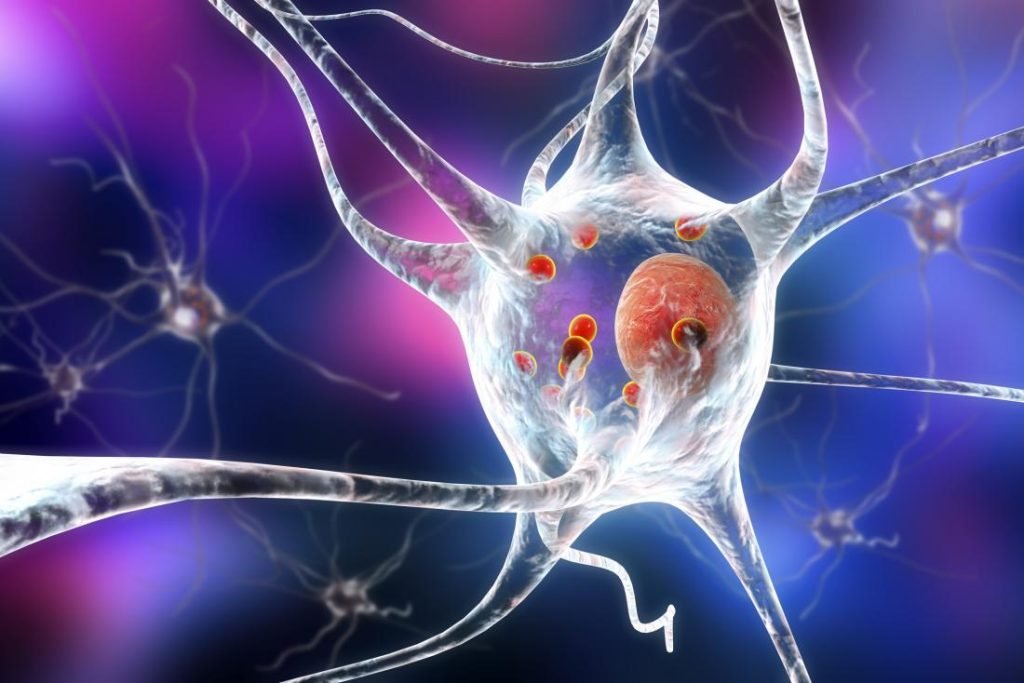
Parkinson’s disease is a neurodegenerative disorder effecting dopaminergic neurons characterized by a range of distinct signs and symptoms. The hallmark signs include tremors, often seen as rhythmic shaking of hands, fingers, or other body parts, along with muscle stiffness,rigidity and postural instability . Individuals with Parkinson’s commonly experience bradykinesia, a slowing down of movements, making everyday tasks challenging. Another notable symptom is postural instability, leading to balance problems and an increased risk of falls. Additionally, Parkinson’s patients may exhibit a shuffling gait, reduced facial expression (referred to as “masked face”), and difficulty with fine motor skills. Non-motor symptoms can include depression, sleep disturbances, and cognitive impairment, further impacting the overall quality of life for those affected by this condition.

In recent research from Lund University, scientists have unveiled a significant breakthrough in the field of neurodegenerative diseases, particularly Parkinson’s disease. This exciting development centers around a newfound blood marker, DOPA decarboxylase (DCC), which promises to revolutionize the diagnosis and treatment of not only Parkinson’s disease but also related disorders with similar symptoms. This article delves into the details of this discovery and its potential implications for early detection and improved patient care.
Parkinson’s Disease and Biomarker Breakthrough
Parkinson’s disease is a debilitating condition that affects millions of people worldwide. One of the biggest challenges in managing this disease is early detection, as it shares clinical symptoms with other neurodegenerative conditions, such as Alzheimer’s disease. However, Lund University researchers have successfully identified a promising biomarker, DOPA decarboxylase (DCC), that may provide a clear path for diagnosing Parkinson’s disease and similar disorders.

The Role of DCC in Identifying Parkinsonian Diseases
The research team at Lund University published their findings in the esteemed journal “Nature Aging,” shedding light on the remarkable potential of DCC. This newly discovered blood marker demonstrates its efficacy in distinguishing Parkinsonian diseases, as its levels were found to be elevated in individuals with Parkinson’s disease and other conditions that involve a dopamine deficiency in the brain. Notably, DCC remained within normal levels for individuals with Alzheimer’s disease, setting it apart as a unique identifier for Parkinson’s and related disorders.
Early Detection and Future Possibilities
One of the most promising aspects of this discovery is its potential for early detection. The researchers noted that DCC levels were elevated in individuals with Parkinson’s many years before they developed any noticeable symptoms. This early warning system could be a game-changer for patients and healthcare providers alike.
To achieve these results, the research team employed advanced protein measurement techniques that allowed them to simultaneously assess thousands of proteins in a small sample. They conducted this extensive analysis on 428 individuals, revealing a clear correlation between damage to the dopamine system in the brain and increased DCC levels. What’s truly groundbreaking is that this biomarker can be measured in the blood, with the most significant elevations observed in Parkinson’s disease cases.
Validation and Reliability
To ensure the reliability of their findings, the researchers verified the correlation in an additional group of 152 individuals. Furthermore, they confirmed the elevated levels of the DCC biomarker in blood by analyzing blood plasma samples from 174 subjects. This extensive validation process underscores the potential of DCC as a dependable diagnostic tool.
READ MORE INTERESTING ARTICLES Animal Crossing: More Than a Game – A Lifeline for Attention deficit hyperactivity disorder ADHD
A Safer and More Accessible Diagnostic Method
In the current landscape of neurodegenerative brain diseases, misdiagnosis is a looming concern. The similarity in symptoms among these conditions often leads to improper treatment. However, the discovery of DCC as a blood marker offers hope for a safer diagnostic approach. Oskar Hansson, a professor of neurology at Lund University and a consultant at Skåne University Hospital, emphasized the importance of finding more reliable and accessible diagnostic tools. This breakthrough could revolutionize the field of neurodegenerative disease diagnosis.
While traditional diagnostic methods rely on costly and complex PET camera examinations to detect damage to the dopamine system in the brain, the use of DCC as a blood marker represents a simpler and more cost-effective approach. This shift toward blood-based diagnosis is not only convenient for patients but also has the potential to reduce the burden on specialized memory clinics, where PET camera examinations are typically performed.
The Future of Diagnosis and Treatment
Dr.Hansson envisions a future where different neurodegenerative brain diseases can be treated even before the symptoms become apparent. Blood markers like DCC are expected to play a pivotal role in identifying the right individuals for early intervention. This is a significant step toward more effective and timely treatment, ultimately improving the quality of life for patients.
In conclusion, Lund University’s groundbreaking discovery of the DOPA decarboxylase (DCC) blood marker offers a ray of hope for individuals affected by Parkinson’s disease and related neurodegenerative disorders. With the potential for early detection and simpler, cost-effective diagnosis, this breakthrough promises to transform the way we approach these conditions. As research in this field progresses, we may be on the cusp of a future where neurodegenerative diseases are identified and treated well before the onset of symptoms, thanks to innovative and accessible blood markers like DCC.
This development marks a significant milestone in the journey towards a better understanding of these conditions and improved patient care.
1 Comment