Insight into Cervical Cancer: Understanding its Internal Dynamics
Background of Cervical cancer
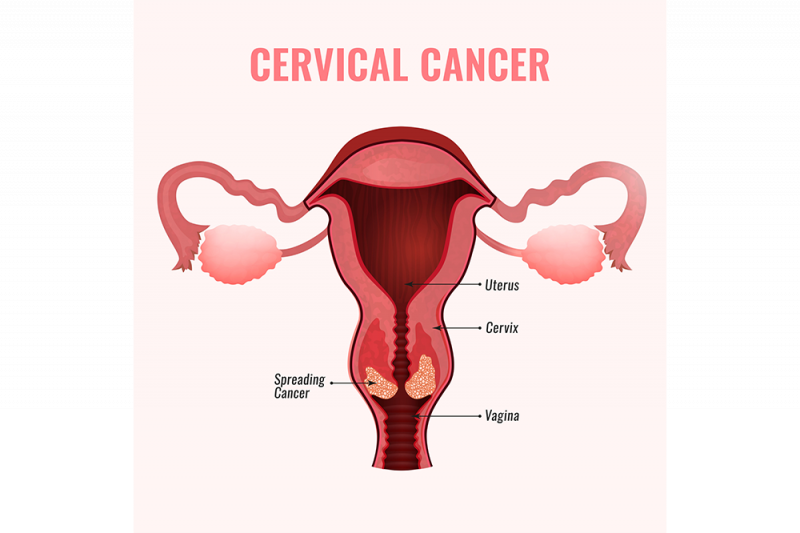
Cervical cancer, a condition that arises from the growth of abnormal cells in the cervix, starts in the lower part of the uterus, connecting to the vaginal canal. Typically, its progression is gradual, marked by a series of cervical tissue changes referred to as dysplasia. During this phase, irregular cells begin to appear in the cervical tissue. If left unaddressed, these irregular cells can evolve into fully-fledged cancer cells, initiating their growth and potential spread into the deeper layers of the cervix and adjacent regions. The most common form of cervical cancer is squamous cell carcinoma, accounting for about 70% of cases, while adenocarcinoma, a less common type representing around 25% of cases, often poses diagnostic challenges due to its origin higher in the cervical region.
Cervical Anatomy and Structure
The cervix, a critical component of the female reproductive system, encompasses two primary sections:

- Ectocervix (Exocervix): This is the outer portion of the cervix that is visible during a gynecological examination. The ectocervix is covered with a layer of thin, flat cells known as squamous cells.
- Endocervix: Situated within the cervix, the endocervix forms a canal connecting the vagina to the uterus. Unlike the ectocervix, the endocervix is lined with column-shaped glandular cells responsible for producing mucus.
The junction where the endocervix and ectocervix meet is called the squamocolumnar junction or transformation zone, which holds particular significance as it marks the starting point for the majority of cervical cancers.
The cervix’s role in the female body is multifaceted:
- Cervical Canal: Within the cervix lies a central canal that serves as a conduit, linking the uterine cavity to the vaginal canal. This canal plays a pivotal role in allowing the passage of menstrual blood from the uterus to the external environment and provides a route for sperm during intercourse.
- Cervical Mucus: Throughout the menstrual cycle, the cervix produces mucus that undergoes changes in consistency. This mucus has various functions, including aiding or impeding the transit of sperm and safeguarding the uterus from potential infections.
- Opening and Closure: The cervix boasts both an external opening, known as the external os, and an internal opening, referred to as the internal os. The external os opens into the vaginal canal, while the internal os leads into the uterine cavity. During childbirth, these openings can expand to facilitate the passage of the baby.
- Barrier Function: In addition to its structural role, the cervix acts as a physical barrier that shields the uterus from external pathogens, such as bacteria and foreign substances. The mucus produced by the cervix contributes to this protective function.
- Menstruation: During the menstrual cycle, the cervix plays a vital role by permitting the flow of menstrual blood from the uterus to the vagina, from where it exits the body.
Understanding the anatomy and functions of the cervix holds paramount importance in women’s health. This knowledge is particularly significant in the contexts of fertility, pregnancy, and the prevention and early detection of cervical conditions, including cancer. Regular gynecological examinations, encompassing procedures like Pap smears and cervical cancer screenings, are essential for monitoring and safeguarding the cervix’s health.
TYPES

Cervical cancer primarily manifests in two main types, each based on the type of cells where the cancer originates:
- Squamous Cell Carcinoma: This is the most prevalent form of cervical cancer, constituting up to 90% of cases. Squamous cell carcinoma initiates in the cells of the ectocervix, the outer part of the cervix, covered with thin, flat squamous cells.
- Adenocarcinoma: Accounting for 10% to 30% of cervical cancer cases, adenocarcinoma begins in the glandular cells of the endocervix, which is the inner part of the cervix. Unlike squamous cell carcinoma, adenocarcinoma arises deeper within the cervical canal, making early detection more challenging in routine screenings like Pap smears.
In some instances, cervical cancer may exhibit features of both squamous cell carcinoma and adenocarcinoma, leading to a classification known as mixed carcinoma or adenosquamous carcinoma. Rarely, cervical cancer may develop in other cervical cell types, presenting unique challenges. However, these instances are infrequent.
It is essential to emphasize that nearly all cases of cervical cancer are associated with high-risk HPV infections. Routine cervical cancer screenings, including Pap smears and HPV testing, play a vital role in early detection and prevention. Additionally, the HPV vaccine offers significant protection against the most common HPV strains that cause cervical cancer.
Sign and Symtoms
- Abnormal vaginal bleeding, such as between periods, after sexual intercourse, or after menopause, can be an early sign of cervical cancer.
- Pelvic pain, which includes persistent discomfort in the pelvis, lower back, or lower abdomen, can be indicative of advanced cervical cancer.
- An increase in vaginal discharge, particularly if it becomes watery, bloody, or has a foul odor, should raise concerns.
- Pain during sexual intercourse, known as dyspareunia, can also be a symptom of cervical cancer.
- Changes in menstrual patterns, such as heavier or longer menstrual periods, may be observed.
- Weight loss, fatigue, and a general feeling of illness can occur in advanced stages of the disease.
It’s important to remember that these signs and symptoms can also be caused by various other conditions unrelated to cancer. Nevertheless, if you experience any of these symptoms, especially if they persist or worsen over time, it is crucial to consult a healthcare professional for a thorough evaluation and appropriate diagnostic tests, such as Pap smears or HPV testing. Early detection and intervention significantly improve the prognosis and outcomes for cervical cancer. Regular cervical screenings and HPV vaccinations are essential for prevention and early detection.
Cervical Cancer Diagnosis:
When it comes to diagnosing cervical cancer, a comprehensive approach is often employed, which includes a range of tests and procedures:
- Initial Assessment: If you present with symptoms or abnormal screening results, your doctor will initiate the diagnostic process. This typically involves discussing your medical history and a physical examination, including a pelvic and rectovaginal exam.
- Imaging Tests: Several imaging tests are used to assess the extent of cervical cancer and potential spread to other areas. These include:
- CT Scan: Providing cross-sectional images of the body to evaluate the disease’s local extent and lymph node involvement.
- MRI (Magnetic Resonance Imaging): Offering detailed images of the pelvis to assess tumor size and involvement of nearby structures.
- PET Scan (Positron Emission Tomography): Detecting distant metastasis by using a radioactive substance that is absorbed by active cancer cells.
- Lymph Node Biopsy: If there’s suspicion of lymph node involvement, a biopsy may be conducted to examine removed lymph nodes for cancer cells.
- Blood Tests: In addition to standard blood tests like CBC and blood chemistry, specific tests may be conducted to assess tumor markers or indicators associated with cervical cancer.
- Visual Examinations: Specialized examinations, such as colposcopy, provide a closer look at the cervix, often accompanied by a biopsy to confirm any abnormalities.
- Cone Biopsy: A surgical procedure to remove a larger, cone-shaped piece of cervical tissue. It can be both diagnostic and therapeutic, used to identify cervical cancer or eliminate precancerous or early-stage lesions.
DIAGNOSIS
Once cervical cancer is diagnosed, the staging process begins, determining the extent of the disease, which is vital for treatment planning. Various procedures, including imaging tests, lab tests, and visual examinations, are employed in the staging process. Additionally, some individuals may choose to seek a second opinion to confirm their diagnosis and treatment plan.
Please note that the choice of specific tests and procedures can vary depending on individual cases and recommendations from healthcare providers.
cervical cancer screening is a highly effective preventive measure that saves lives by detecting precancerous cervical cell changes before they develop into cancer. Although screening offers substantial benefits, it’s essential to be aware of potential risks and to understand when and how to get screened. Here’s a comprehensive guide to cervical cancer screening, including when to get screened, who should be screened, and where to access these crucial tests for precaution:
The Power of Cervical Cancer Screening: Cervical cancer screening is a vital tool in healthcare that can significantly reduce the risk of developing cervical cancer. Regular screening detects abnormal cervical changes early, increasing the chances of preventing cervical cancer and saving lives.
Potential Risks of Harm: While cervical cancer screening offers many advantages, it is not without potential drawbacks. It’s important to discuss these with your healthcare provider before undergoing screening:
- Unnecessary Follow-up Tests and Treatment: In some cases, screening may detect conditions that would not have caused harm, leading to unnecessary follow-up tests and treatments. Current screening guidelines aim to minimize the risk of treating harmless conditions.
- False-Positive Test Results: False-positive results can create anxiety and may lead to additional tests and procedures when no precancer or cancer is present. This can include colposcopy, cryotherapy, or loop electrosurgical excision procedures, which carry their own set of risks.
- False-Negative Test Results: On the flip side, false-negative results may occur, indicating normal test results when cervical precancer or cancer is present. This can lead to delayed medical care, even if symptoms are present.

Types of Cervical Cancer Screening: There are three primary methods for cervical cancer screening:
- HPV Test: This test checks for infection with high-risk HPV types that can lead to cervical cancer.
- Pap Test (Pap Smear): Pap tests collect cervical cells to identify changes caused by HPV. They can detect precancerous cells and cervical cancer cells, as well as non-cancerous conditions like infections or inflammation.
- HPV/Pap Cotest: This combines both the HPV test and Pap test to check for high-risk HPV and cervical cell changes.
When to Get Screened: Screening recommendations depend on age and health history. Here are some general guidelines:
- Age 21-29: Begin with a Pap test every 3 years.
- Age 30-65: Options include an HPV test every 5 years, an HPV/Pap cotest every 5 years, or a Pap test every 3 years.
- Age 65 and Older: Discuss with your healthcare provider if screening is still necessary, based on your history.
Exceptions to Screening Guidelines: In some cases, more frequent screening may be recommended, such as if you have HIV, a weakened immune system, or were exposed to diethylstilbestrol (DES) before birth. Recent abnormal screening results or a history of cervical cancer may also warrant more frequent screening.
Where to Get Screened: Cervical cancer screening is widely accessible and offered by:
- Primary care providers
- Clinics and health centers
- Women’s health services
- Organizations like Planned Parenthood
- State or local health departments
- The National Breast and Cervical Cancer Early Detection Program
- NCI’s Cancer Information Service
Screening is typically done during a pelvic exam, which is a brief and straightforward procedure. It involves a speculum to gently open the vagina, followed by the collection of cervical cell samples using a brush or spatula.
Regular cervical cancer screening, in line with your healthcare provider’s guidance, is a powerful step toward maintaining your health and well-being. It not only offers peace of mind but also plays a significant role in preventing and treating cervical cancer.
Cervical Cancer Stages
Cervical Cancer Types and Stages
Cervical cancer is a significant health concern, but it can be better understood by breaking it down into its types and stages:
Types of Cervical Cancer:
- Squamous Cell Carcinoma: This is the most common type of cervical cancer, accounting for approximately 70-90% of cases. It starts in the thin, flat cells (squamous cells) lining the cervix.
- Adenocarcinoma: Accounting for about 10-30% of cervical cancer cases, adenocarcinoma develops in the glandular cells of the cervix, which produce mucus.
- Adenosquamous Carcinoma: This is a less common type of cervical cancer that exhibits features of both squamous cell carcinoma and adenocarcinoma.
- Small Cell Carcinoma: A rare and aggressive type of cervical cancer, small cell carcinoma starts in the nerve cells or hormone-producing cells in the cervix.
- Neuroendocrine Tumors: These tumors arise from hormone-producing cells and are a rare type of cervical cancer.
Stages of Cervical Cancer:
Cervical cancer is staged from 0 to IV, indicating the extent of its spread:
- Stage 0 (Carcinoma in Situ): The cancer is only in the top layer of cells lining the cervix and has not invaded deeper tissues.
- Stage I: Cancer is confined to the cervix.
- IA: A very small amount of cancer that can only be seen under a microscope.
- IB: Cancer is visible to the naked eye but is still confined to the cervix.
- Stage II: Cancer has spread beyond the cervix but not to the pelvic wall or the lower third of the vagina.
- IIA: Cancer involves the upper two-thirds of the vagina but not the pelvic wall.
- IIB: Cancer has invaded the parametrial tissues but not the pelvic wall.
- Stage III: Cancer has spread to the lower third of the vagina, may have invaded the pelvic wall, and can cause kidney problems.
- IIIA: Cancer involves the lower third of the vagina but not the pelvic wall.
- IIIB: Cancer extends to the pelvic wall or causes kidney problems.
- Stage IVA: Cancer has spread to adjacent organs, such as the bladder or rectum.
- Stage IVB: Cancer has spread to distant organs or lymph nodes in other parts of the body.
The stage of cervical cancer helps doctors determine the appropriate treatment plan, which may include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of these treatments. Regular screenings and early detection play a crucial role in improving outcomes for individuals diagnosed with cervical cancer.
Cervical Cancer Treatment
The treatment of cervical cancer encompasses various approaches tailored to the patient’s unique circumstances. Your medical team collaborates with you to formulate a comprehensive treatment plan, taking into account factors such as the cancer’s stage, your overall health, and your preferences. Your treatment plan includes essential information about your cancer, the objectives of treatment, treatment options, potential side effects, and the expected duration of the treatment.
If concerns about fertility are on your mind, it’s advisable to engage in a conversation with your medical team before treatment commencement to gain insight into how treatment may impact your fertility. To explore fertility preservation choices and seek support, refer to the section on Fertility Issues in Girls and Women with Cancer.
For a more detailed breakdown of treatment options according to the stage of cervical cancer, please see the section on Cervical Cancer Treatment by Stage.
Should you be interested in learning about treatment during pregnancy, comprehensive information is available in the section on Cervical Cancer Treatment during Pregnancy.
Surgery
Surgery, also known as an operation, is occasionally employed as a means to treat cervical cancer. The type of surgery chosen depends on the specific location of the cancer. The following surgical procedures may be utilized:
- Cold Knife Conization: Involves the removal of a cone-shaped section of cervical tissue using a scalpel. In some cases, this procedure can completely eliminate the cancer. It is typically performed in a hospital setting under general anesthesia.
- Sentinel Lymph Node Biopsy: This procedure extracts the sentinel lymph node during surgery. The sentinel lymph node, the first lymph node to receive lymphatic drainage from the primary tumor, is a likely site for cancer spread. After identifying the sentinel lymph node using a radioactive substance or dye, a pathologist examines the tissue for cancer cells. If cancer cells are found, additional lymph nodes are removed through a separate incision, termed lymph node dissection.
- Hysterectomy: Hysterectomy involves the removal of the uterus. In treating cervical cancer, the cervix, and sometimes surrounding structures are also removed. Various types of hysterectomy may be employed, including total vaginal, total abdominal, or total laparoscopic hysterectomy. Radical hysterectomy and modified radical hysterectomy are more extensive procedures that may involve the removal of additional tissues and organs, such as the ovaries and nearby lymph nodes.
- Radical Trachelectomy: This procedure removes the cervix, nearby tissue, and the upper part of the vagina. Lymph nodes may also be removed. After cervix removal, the uterus is attached to the remaining part of the vagina to preserve fertility.
- Bilateral Salpingo-Oophorectomy: This surgery removes both ovaries and fallopian tubes, a measure taken when cancer has spread to these organs.
- Total Pelvic Exenteration: A more extensive surgery that removes the lower colon, rectum, bladder, cervix, vagina, ovaries, nearby lymph nodes, and creates artificial openings for urine and stool to exit the body.
Radiation Therapy
Radiation therapy employs high-energy X-rays or other forms of radiation to either eliminate cancer cells or inhibit their growth by damaging their DNA. There are two primary types of radiation therapy: external radiation therapy and internal radiation therapy, also known as brachytherapy.
Both external and internal radiation therapy play crucial roles in treating cervical cancer and may be used to alleviate symptoms and improve the quality of life in individuals with advanced cervical cancer.
Chemotherapy
Chemotherapy, involving the use of drugs to impede the growth or induce the death of cancer cells, can be administered alone or in combination with other treatments. Several chemotherapy drugs, such as cisplatin, carboplatin, gemcitabine, and others, are employed in treating cervical cancer.
Targeted Therapy
Targeted therapy utilizes drugs or substances to obstruct specific molecules and pathways associated with cancer cell growth and proliferation. Notable targeted therapies for cervical cancer include bevacizumab and tisotumab vedotin.
Immunotherapy
Immunotherapy enhances the body’s immune system to combat cancer. Biomarker tests can determine the suitability of certain immunotherapy drugs. Pembrolizumab is an immunotherapy drug used for specific cervical cancer patients with the PD-L1 biomarker.
Clinical Trials
Clinical trials are research studies designed to advance existing treatments or explore new ones for cancer patients. Participating in a clinical trial may be an option for some individuals. NCI-supported clinical trials can be found using the clinical trial search.
Follow-Up Testing During and After Treatment
Tests conducted for diagnosis and staging purposes may be repeated during treatment to assess its efficacy. These test results inform decisions regarding the continuation, modification, or cessation of treatment.
After treatment, periodic follow-up tests are performed to monitor any changes in your condition and the possibility of cancer recurrence. Be vigilant for signs such as vaginal bleeding, abdominal or leg pain, swelling in the leg, urinary difficulties, changes in bowel movements, persistent cough, and fatigue. The frequency of follow-up tests for cervical cancer is typically every 3 to 4 months for the first 2 years, followed by semi-annual check-ups, including a health history review and a physical examination to detect any signs of recurrent cervical cancer or late effects of treatment. Pap tests may be conducted during these visits as needed.
